Abstract

Background: Despite recent advances in the treatment of relapsed/refractory multiple myeloma (RRMM), novel agents are needed to improve outcomes. Ibrutinib (ibr) is a first-in-class, once-daily oral inhibitor of Bruton's tyrosine kinase (BTK), an enzyme implicated in the growth and survival of multiple myeloma (MM) cells, providing the rationale for evaluating BTK inhibitors in MM (Yang Cancer Res 2015). Study PCYC-1119 (NCT01962792) is an ongoing phase 1/2b study of ibr + carfilzomib (CFZ) ± dexamethasone (dex). Initial phase 1 data established ibr 840 mg daily (qd) with CFZ 20/36 mg/m2 twice weekly (biw) + dex 20 mg biw as the recommended phase 2b dose (RP2D) (Chari ASH 2015).
Methods: Eligible patients (pts) received ≥2 prior therapies, including bortezomib (BTZ) and an immunomodulatory drug (IMiD), and had either no response or documented disease progression following the most recent treatment. The objectives of the phase 2 portion, in which pts received the RP2D of ibr with CFZ + dex, include overall response rate (ORR) and median progression-free survival (PFS).
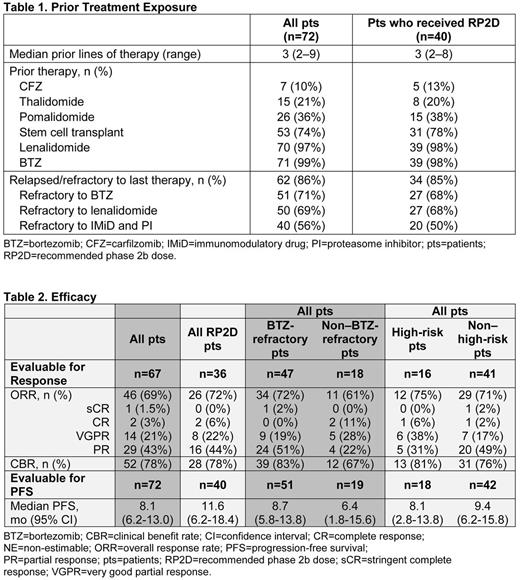
Results: As of May 1, 2017, 72 pts had received ibr combined with CFZ ± dex across multiple dose levels; 40 of these pts had received the RP2D. Among all 72 pts, the median age was 63 years (range, 34-83) and the median time from diagnosis was 4.5 years (range, 0.5-25.3), consistent with what was previously reported in the phase 1 portion. Fluorescence in situ hybridization (FISH) performed locally identified that 10/72 (13.9%) and 9/72 (12.5%) pts had del(17)(p13) and t(4;14), respectively. Gene expression profiling (GEP) in an initial subset of 18 phase 2 pts revealed 8 (44%) pts as high-risk. Prior treatment exposure is summarized in Table 1. Duration of treatment ranged from 0 to 29 months, and 15 pts remain on treatment.
Of the 40 pts who received the RP2D, 36 were evaluable for response (Table 2). The ORR was 72% and PFS was 11.6 mos. Subgroup analysis revealed favorable outcomes for BTZ-refractory (n=24, ORR 83% and PFS 13.8 mos) and high-risk patients (n=11, ORR 82% and PFS 9.8 mos). Since patients in the phase 1 dose escalation portion of the study received biologically active doses of all agents, the outcomes in the combined population (n=72) were also evaluated. The ORR and PFS for BTZ-refractory compared to non-BTZ refractory patients were 72% and 8.7 mos vs. 61% and 6.4 mos, respectively. For high-risk vs. non-high-risk patients, the ORR and PFS were 75% and 8.1 mos vs. 71% and 9.4 mos, respectively.
The tolerability of the combination at the RP2D is consistent with safety observed in phase 1. Among the 40 RP2D pts, the most common (occurring in >25% of pts) all-grade nonhematologic adverse events (AEs) were nausea (50%), diarrhea (48%), fatigue (38%), cough (35%), hypertension (28%), gastroesophageal reflux (28%), and insomnia (28%). Grade ≥3 hematologic AEs occurring in >5% of pts included anemia (15%), thrombocytopenia (13%), and neutropenia (8%). Grade ≥3 nonhematologic AEs occurring in ≥10% of pts were hypertension (18%), pneumonia (13%), diarrhea (10%), and hyperglycemia (10%).
Among the 72 total pts, 36 pts experienced treatment-related serious AEs. Twenty-seven pts discontinued study treatment due to progressive disease; an additional 13 pts discontinued due to investigator or pt decision. While 16 pts (22%) of all 72 pts discontinued due to an AE, only 4 pts (10%) at RP2D did so, with 2 events related to psychiatric disorders (confusional state, depression), 1 gastrointestinal hemorrhage, and 1 event of pneumonia. For pts receiving the RP2D to date, there has been one report of cardiac flutter (grade 1) that resolved with no intervention and was attributed to CFZ. Updated data will be presented.
Conclusions: These data further support the RP2D of ibr 840 mg qd with CFZ 20/36 mg/m2 biw + dex 20 mg biw as an option for the treatment of RRMM. AEs were manageable, and the ORR of 72%, including 2 complete responses and 8 very good partial responses, is promising in this heavily refractory population. Importantly, the addition of ibrutinib to CFZ and dex may overcome the adverse prognosis associated with bortezomib resistance. The outcomes of high-risk patients are encouraging and warrant further study.
Chari: Array BioPharma: Consultancy, Membership on an entity's Board of Directors or advisory committees, Other: Travel, Research Funding; Pharmacyclics: Research Funding; Novartis: Consultancy, Membership on an entity's Board of Directors or advisory committees, Other: Travel, Research Funding; Janssen: Consultancy, Membership on an entity's Board of Directors or advisory committees, Other: Travel, Research Funding; Bristol-Myers Squibb: Consultancy, Other: Research funding (to AC's institution); travel, Research Funding; Amgen: Consultancy, Membership on an entity's Board of Directors or advisory committees, Other: Travel, Research Funding; Celgene: Consultancy, Membership on an entity's Board of Directors or advisory committees, Other: Travel, Research Funding; Biotest: Other: Research funding (to AC's institution), Research Funding; Acetylon Pharmaceuticals: Other: Research funding (to AC's institution); Onyx: Research Funding; Millennium: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding. Girnius: Celgene: Speakers Bureau; Takeda: Other: Travel; consulting/advisory role on steering committee, Speakers Bureau. Chhabra: Cardinal Health: Honoraria; Incyte: Honoraria. Gasparetto: Janssen, BMS, Celgene: Other: Travel, accommodations, or other expenses paid or reimbursed; Janssen, BMS, Celgene, Takeda: Honoraria; Janssen, BMS, Celgene: Consultancy; Celgene: Research Funding. Lunning: Epizyme: Consultancy; Pharmacyclics: Consultancy; Celgene: Consultancy; Gilead: Consultancy; Genentech: Consultancy; Juno: Consultancy; Spectrum: Consultancy; TG Therapeutics: Consultancy; AbbVie: Consultancy; BMS: Consultancy; Onyx: Consultancy. Matous: Amgen: Speakers Bureau; Celgene: Other: Myeloma Advisory Board, Speakers Bureau. Niesvizky: Amgen: Consultancy; Janssen: Consultancy; BMS: Consultancy; Celgene: Consultancy. Shustik: Takeda: Honoraria; Amgen: Honoraria; Celgene: Honoraria. Stuart: Bayer: Research Funding; Cantex: Research Funding; Incyte: Research Funding; Novartis: Research Funding; MedImmune: Research Funding; Celator/Jazz: Research Funding; ONO: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Agios: Research Funding; Astellas: Research Funding; Seattle Genetics: Research Funding; Amgen: Consultancy, Honoraria; Pharmacyclics LLC, an AbbVie Company: Research Funding; Sunesis: Consultancy, Honoraria, Other: Travel Support, Research Funding. Lih: AbbVie: Equity Ownership; Pharmacyclics: Employment. Lee: Pharmacyclics: Employment; AbbVie: Equity Ownership. Salman: AbbVie: Equity Ownership; Pharmacyclics: Employment. Graef: Pharmacyclics: Employment, Patents & Royalties: oncology; AbbVie: Equity Ownership. Valent: Takeda: Speakers Bureau; Celgene Corporation: Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal